Bio-Identical HRT: It matters
As I approach my 47th birthday, I've noticed subtle yet unmistakable shifts in my body—irregular sleep patterns, mood swings that catch me off guard, and a nagging fatigue that no amount of coffee seems to fix. These changes have sparked my curiosity and led me down a rabbit hole of personal research into perimenopause and hormonal fluctuations. What started as a quest for answers about my own symptoms has revealed a wealth of insights on how estrogen and progesterone levels begin to wane unevenly during this transitional phase, often leading to overlooked issues like anovulatory cycles even with seemingly regular periods. I've delved into studies on bioidentical hormones versus synthetics, the critical balance these hormones maintain for everything from bone density to brain health, and the surprising prevalence of progesterone drops in women my age that can manifest in ways we don't immediately connect to hormones. Here's what I've uncovered so far, and why it's empowering me to take charge of my well-being.
The balance between the hormones matters
Maintaining a physiological balance of both estrogen and progesterone is essential for preserving the health and function of tissues throughout the body, extending far beyond reproductive roles. These hormones work synergistically. Estrogen primarily helps regulate inflammation, support vascular integrity, and inhibit excessive tissue breakdown, while progesterone promotes repair, stabilization, and new tissue formation.
In joints, estrogen maintains synovial fluid production and collagen integrity to reduce stiffness and friction, while progesterone supports cartilage health and reduces inflammatory joint pain often reported to improve with balanced therapy.
For the brain, estrogen protects neurons, enhances synaptic plasticity, and supports cognitive functions like memory and focus, potentially delaying age related decline. Progesterone complements this by modulating mood, reducing neuroinflammation, and aiding in brain repair mechanisms.
In the cardiovascular system, estrogen promotes vasodilation, maintains healthy cholesterol balance, and keeps blood vessels flexible to lower heart disease risk post menopause. Progesterone helps regulate blood pressure and supports endothelial function without the adverse effects seen with some synthetic alternatives.
For bones, estrogen slows excessive resorption to preserve density, while progesterone actively stimulates osteoblast activity for new bone formation. Together they create a balanced remodeling process that counters the accelerated loss seen in estrogen dominant or deficient states.
When levels decline unevenly during menopause, tissues lose this protective harmony, increasing vulnerability to osteoporosis, cognitive changes, joint discomfort, and cardiovascular issues.
Bioidentical hormone approaches that restore a natural estrogen progesterone ratio aim to mimic this lifelong physiological partnership, helping sustain tissue resilience, vitality, and long term wellness across these critical systems.
Why You might be low on Progesterone even if you are still cycling normally
During the ovulation phase of a woman's menstrual cycle, progesterone production ramps up significantly after an egg is released from the ovary; the ruptured follicle transforms into the corpus luteum, a temporary endocrine structure that secretes progesterone to prepare the uterine lining for potential pregnancy, maintaining elevated levels for about 10-14 days until it either sustains a pregnancy or regresses if no implantation occurs. However, in cases of ovulation failure—also known as anovulation—a woman may experience a sharp drop in progesterone because no corpus luteum forms, even if she continues to have regular menstrual bleeding that mimics a normal period due to estrogen-driven buildup and shedding of the uterine lining without actual egg release. This phenomenon is surprisingly common, with studies indicating that up to 30-50% of women in their late 30s may unknowingly experience non-ovulatory cycles as they approach perimenopause, often attributing the irregularity to stress or other factors rather than hormonal shifts. A resulting decline in progesterone can trigger a cascade of symptoms that many women fail to connect to this underlying cause, including intensified PMS, mood swings, anxiety, sleep disturbances, breast tenderness, bloating, and even heavier or irregular bleeding, which can erode quality of life and mimic other health issues if left unaddressed.
Recent Research Trends around the safety of HRT for even women with a risk of Breast Cancer
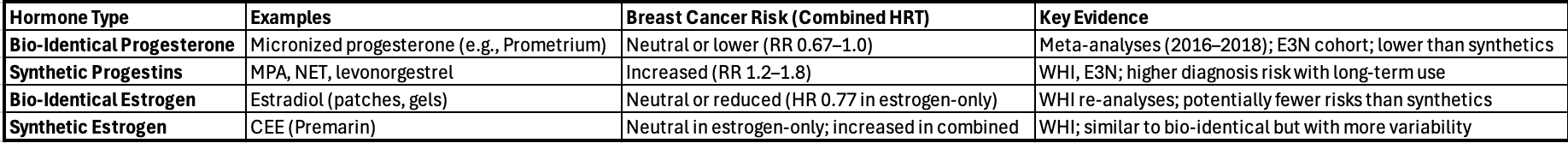
Recent studies primarily from 2016 to 2025, with ongoing analyses of large cohorts like WHI and E3N, have increasingly differentiated between bio identical hormones such as micronized progesterone and estradiol derived from plants and structurally identical to human hormones, and synthetic versions such as progestins like medroxyprogesterone acetate and norethisterone, and estrogens like conjugated equine estrogens.
The focus is often on combined hormone replacement therapy, where the progestogen component appears to drive much of the risk difference.
Bio identical options are generally associated with lower or neutral breast cancer risk compared to synthetics, though evidence is stronger for progesterone than for estrogen.
Below is a summary of major findings.
Progesterone Bio Identical vs Synthetic Progestins
Most research highlights a lower breast cancer risk with bio identical progesterone, often micronized, compared to synthetic progestins when combined with estrogen.
This is based on meta analyses and large cohort studies.
A 2016 systematic review and meta analysis covering 86,881 women across multiple trials found that estrogen plus bio identical progesterone was linked to a significantly lower breast cancer risk with a relative risk of 0.67 compared to estrogen plus synthetic progestins like MPA.
The French E3N cohort study of 80,377 postmenopausal women followed from 1990 to 2002 with updates through 2025 showed that estrogen plus bio identical progesterone or dydrogesterone had a lower invasive breast cancer risk with relative risk between 0.9 and 1.0 than estrogen plus other synthetic progestagens which showed relative risk up to 1.8.
A 2018 systematic review on micronized progesterone analyzing 14 trials reported no increased breast cancer risk with estrogen plus micronized progesterone, while synthetics like MPA or NET were associated with higher risks between relative risk 1.2 and 1.5.
2025 analyses from the Womens Health Initiative long term follow up confirmed that combined HRT with synthetic progestins increased breast cancer incidence, but bio identical alternatives showed neutral or reduced effects in subgroup re analyses.
Estrogen Bio Identical vs Synthetic Estrogens
Evidence here is less definitive, with bio identical estradiol often showing similar or slightly better safety profiles than synthetics like CEE, especially in estrogen only HRT.
WHI follow ups through 2025 indicate that estrogen only HRT using synthetic CEE actually reduced breast cancer risk with a hazard ratio of 0.77 in women post hysterectomy, with no clear increase even after 20 years.
However, bio identical estradiol is argued to be even safer due to more precise dosing and fewer metabolites, though direct head to head trials are limited.
A 2025 review emphasized that bio identical estradiol alone does not elevate risk and may protect against breast cancer in some contexts, unlike broader estrogen categories that include synthetics.
Combined with progestogens, the estrogen type matters less than the progestogen. Bio identical estradiol plus progesterone shows lower risks than CEE plus MPA.
Comparison of Bio Identical vs Synthetic Hormones in HRT
Comparisons of Bio Identical vs Synthetic Hormones
Important Caveats and Consensus
Compounded bio identical hormone replacement therapy is cautioned by some sources because compounded custom mixed hormones lack large scale FDA regulated trials and may have inconsistent dosing. This could potentially mirror synthetic risks if not monitored. FDA approved bio identical hormones such as micronized progesterone have stronger evidence.
Overall risk shows that estrogen only HRT either bio identical or synthetic is generally safer for breast cancer than combined therapies. Risks are higher in women over 60 or with long term use greater than five years.
Mechanisms suggest that bio identical progesterone may avoid promoting cell proliferation in breast tissue, unlike synthetics that can bind differently to receptors.
Expert groups such as the North American Menopause Society in guidelines from 2022 to 2025 recommend individualized assessment, often favoring bio identical options for symptomatic women at higher risk, while noting that more randomized trials are still needed for definitive comparisons.
As I continue navigating this new chapter at 47, I’m committed to staying curious and proactive—diving deeper into the latest studies, tracking my symptoms with greater intention, and having open, informed conversations with my doctor. In this era of personalized medicine, I feel empowered knowing we can tailor solutions—whether through lifestyle adjustments, bioidentical hormone options, or other targeted approaches—to fit my unique biology, symptoms, and goals rather than following a one-size-fits-all script. It’s an ongoing process, not a quick fix, but every piece of research I explore and every discussion I have brings me closer to feeling more like myself again. I’m excited to keep learning, advocating for what my body needs, and sharing what I discover along the way.