The Mouth-Body Connection: Why Dental Health Shapes Your Whole Body and How to Take Evidence-Based Action to Maintain it
Your oral health will impact the rest of your body’s health
The concepts in this article are pulled from two youtube videos: — “Germs and the Big Lie” by Dr. Paul Mason and the Dr. Praep Jam Nadas interview —and explains why dental health is critical to the health of the entire body, with citations at the bottom.
We tend to think of oral health as something cosmetic — white teeth, fresh breath, no cavities. But science is revealing a much deeper truth: your mouth is a mirror of your body’s health. The bacteria that live between your teeth and gums can influence your heart, brain, metabolism, and even your risk for cancer. What’s happening in your mouth doesn’t stay there — it travels throughout your bloodstream.
Let’s explore how this happens and why keeping your teeth clean may be one of the simplest ways to protect your life.
The Hidden Highway Between Mouth and Body
Your mouth is the front door to your body’s ecosystem. Every time you chew, brush, or even swallow, tiny microbes — bacteria, viruses, and fungi — can enter the bloodstream through microscopic tears in the gums.
As Dr. Paul Mason explains, when we brush our teeth, we can release oral bacteria like Porphyromonas gingivalis into the blood — the same bacteria found inside atherosclerotic plaques of people who suffer heart attacks. One study even found bacteria in the blood of 38% of children just from toothbrushing. That means a daily habit as innocent as brushing can let mouth microbes travel directly to your arteries, heart, and brain.
The mouth’s ecosystem, when healthy, protects you. But when gum disease develops — when gums are inflamed and pockets of plaque form — it becomes a launchpad for infection and chronic inflammation throughout the body.
When Oral Bacteria Invade the Heart
In 2011, scientists examined 42 atherosclerotic plaques removed during surgery and found bacterial DNA in every single one. That’s not coincidence — that’s connection. A 2014 study confirmed it, showing that 95% of arterial biopsies from people with gum disease contained bacterial DNA from the same microbes found in the mouth.
Animal studies reveal how direct the link is: pigs injected with P. gingivalis, a bacteria that causes gum disease, developed artery-clogging plaques within weeks. These plaques looked identical to human heart disease.
This means that the very same bacteria responsible for bleeding gums and bad breath may also trigger the buildup of fatty, inflamed plaques in your arteries — the root cause of heart attacks and strokes.
Dr. Mason notes that patients admitted to hospitals with bacterial infections in their blood are 18 times more likely to suffer a heart attack or stroke within 30 days. That’s an 1,800% increase in risk — far higher than smoking.
The Inflammation Link: From Gums to Arteries
Dr. Praep Jam Nadas, a cardiologist who’s treated over 30,000 heart patients, puts it simply: heart disease starts with inflammation.
A plaque in an artery doesn’t cause a heart attack until it cracks — like a pimple bursting — triggering a blood clot. What causes that crack? Inflammation. And inflammation comes from your body constantly reacting to something foreign, something irritating your system day after day.
One of those irritants can be bacterial endotoxins from gum disease. These tiny bacterial fragments travel through the blood, triggering the same immune alarms that cause artery walls to swell, thicken, and eventually rupture.
So when your gums are inflamed, your arteries likely are too.
The Microbial Fingerprints of Disease
The same bacteria found in gum disease and dental infections — P. gingivalis, Fusobacterium nucleatum, Treponema denticola — have been detected in tumors, arterial plaques, and even the brain tissue of Alzheimer’s patients.
Here’s what the research shows:
Heart disease: 95% of atherosclerotic plaques contain bacterial DNA from oral pathogens.
Cancer: Fusobacterium nucleatum is found in many colorectal cancers and is believed to accelerate tumor growth.
Brain disease: P. gingivalis DNA and its toxic enzymes have been found in the brains of people with Alzheimer’s disease, suggesting that chronic gum infections could trigger neuroinflammation.
Arthritis and autoimmune disorders: Oral bacteria can prime the immune system to attack healthy tissues, worsening systemic inflammation.
In other words, the bacteria between your teeth don’t just stay in your mouth — they become your body’s uninvited guests everywhere.
The Blood Sugar Connection
Dr. Nadas’ decades of cardiology experience also show that metabolic dysfunction — especially high insulin levels and insulin resistance — accelerates inflammation and plaque formation.
What’s fascinating is that the same metabolic environment that promotes gum disease — high sugar intake, frequent snacking, processed carbs — also feeds oral bacteria and raises systemic insulin. Elevated insulin makes blood “stickier,” encourages clotting, and causes smooth muscle growth in arteries, setting the stage for blockages.
So your diet doesn’t just feed you — it feeds your bacteria too.
The Bigger Picture: Your Mouth Is a Map
Your oral health is an early warning system for what’s happening inside your body.
Bleeding gums? That’s systemic inflammation. Receding gum lines? Possible metabolic stress. Chronic bad breath? Bacterial imbalance.
It’s time we stop thinking of dentistry as separate from medicine. The mouth is where whole-body health begins. The bacteria that grow there can either support your vitality or silently seed disease.
So the next time you pick up your toothbrush, remember: you’re not just cleaning your smile — you’re protecting your heart, your brain, and your future.
Sources:
Dr. Paul Mason, Germs and the Big Lie — correlations between oral pathogens and cardiovascular disease
Dr. Praep Jam Nadas, interview on inflammation, insulin, and plaque formation
Part 2: This section of this article is based on the research on how to maintain our oral health.
🦷 The Balanced Mouth: How to Keep Your Teeth, Gums, and Microbiome Healthy — Without Breaking the Bank
We’ve been taught for decades that oral care means sterilizing our mouths. Rinse, foam, kill — repeat.
But your mouth isn’t a war zone. It’s an ecosystem.
Inside live billions of microbes — some harmful (P. gingivalis, S. mutans), many helpful (Lactobacillus reuteri, S. sanguinis). The health of your gums, arteries, even your brain, depends on keeping these microbial citizens in balance.
So how do you protect enamel, stop inflammation, and honor your microbiome without spending hundreds on fancy rinses and probiotic lozenges?
Let’s compare what really works — biologically, financially, and ecologically.
🧬 1. The Three Oral-Care Philosophies
Approach Goal Typical Tools Antiseptic + Rebuild Kill harmful bacteria, then recolonize with probiotics CHX/CPC mouthwash, stannous-fluoride toothpaste, L. reuteri lozenges Natural Balance Preserve beneficial flora; use gentle biofilm control Oil pulling, green-tea rinses, xylitol, thorough brushing Biomimetic Remineralization Restore enamel structure and harmony Nano-hydroxyapatite toothpaste, probiotics, mild rinses
Each works — but each has trade-offs in cost, speed, and ecological harmony.
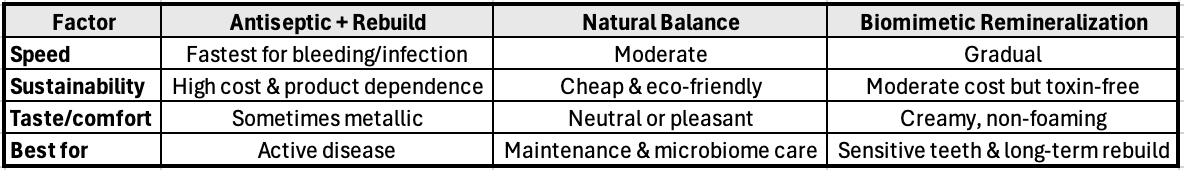
⚖️ 2. Quick Outcome Comparison
Quick comparison of the strategies
💵 3. Cost Breakdown (3 Months)
Quick Cost breakdown
🦠 4. Microbiome Impact Summary
Quick impact summary
🧾 5. Protocol Options
A. Reset & Rebuild (for inflamed gums)
Duration: 2–4 weeks
Cost: ≈ $60–80
Goal: Stop bleeding + rebalance microbes
Morning
Brush with stannous-fluoride toothpaste (2 min)
CHX rinse (30 s, spit, don’t swallow)
Wait 1 hr → dissolve one L. reuteri Prodentis lozenge
Evening
Brush again with stannous fluoride
CPC rinse or green-tea rinse if CHX cycle is complete
Optional: Oil pulling (10 min) before brushing
After 2 weeks: stop CHX; continue CPC + L. reuteri for 1 month.
B. Natural Balance Maintenance
Duration: Ongoing
Cost: ≈ $15–25 per quarter
Morning
Oil pull (10 min while showering) → spit in trash
Brush with nano-hydroxyapatite toothpaste
Interdental clean
Evening
Brush again with n-HAp paste
Green-tea rinse (steep bag 5 min, cool, swish 1 min)
Xylitol gum/lozenge after meals (6–10 g daily)
Benefits: Supports microbiome diversity, gentle plaque control, budget friendly.
C. Hybrid Microbiome Optimizer
Duration: Ongoing, cycle seasonally
Cost: ≈ $30–40 per quarter
Hybrid timing approach
⏱ 6. Timing Tips
Fully naturally timing
🌱 7. Trade-Off Insights
Look at the trade offs
🧭 8. Integral Recommendation
Think in seasons, not products.
Spring / Reset: 2-week antiseptic phase if you have inflammation.
Summer / Growth: Switch to nano-hydroxyapatite and green-tea rinses.
Autumn / Balance: Keep xylitol and occasional oil pulling to sustain flora.
Winter / Recovery: Add L. reuteri after antibiotics or stress.
Your mouth, like a garden, needs pruning, feeding, and rest in rhythm — not daily warfare.
🪴 9. The $20 Mouth vs. The $300 Mouth
Lets look at the numbers
🧩 10. Closing Thought
Your teeth aren’t just bone—they’re living crystals in conversation with your microbes.
Instead of fighting them, learn to host them well.
Brush with intention, clean between, swish with kindness, and let your mouth become what nature intended: a self-healing ecosystem.